The Liquid Biopsy Hematology Profile uses cell-free DNA (cfDNA) for detecting abnormalities in hematologic diseases and for monitoring minimal residual disease (MRD). The Liquid Biopsy Hematology Profile is designed and offered to reduce the need for a bone marrow biopsy. It is highly useful for patients presenting with cytopenia and to rule out MDS/CMML, MPN or other hematologic neoplasms. It can also be used for monitoring patients with hematologic neoplasms and therapeutic response. Based on multiple studies, cfDNA can be more accurate in detecting abnormalities in bone marrow than an actual bone marrow biopsy. Bone marrow biopsy might be limited to site of the biopsy, while the cfDNA reflects abnormalities in the entire body. Furthermore, based on our investigation, plasma is enriched by cancer-specific DNA/RNA due to the high turnover of tumor cells as compared with normal cells. This test is recommended for the diagnosis and follow up of:
Myelodysplastic syndrome (MDS)/Chronic myelomonocytic leukemia (CMML): To determine if the patient has reactive cytopenia and to distinguish between CHIP (Clonal Hematopoiesis of Indeterminate Potential) or CCUS (Clonal Cytopenia of Unknown Significance) and MDS.
VEXAS Syndrome: Recently described VEXAS (vacuoles, E1 enzyme, X-linked, autoinflammatory, somatic) is caused by mutations in the UBA1 gene. This is an adults-onset fatal disease that may present as myelodysplastic syndrome, aplastic anemia or multiple myeloma, but characterized by fevers, low white cell count, vacuoles in bone marrow cells, dysplastic bone marrow, pulmonary inflammation, chondritis, and vasculitis. Detecting the presence of mutations in the UBA1 gene is the only way for confirming the diagnosis of this syndrome.
Acute Myeloid Leukemia (AML): To confirm diagnosis of AML and helps in determining eligibility for treatment with FLT3 and IDH1/2 inhibitors and evaluate minimal/measurable residual disease (MRD). It is particularly useful for pediatric and elderly patients.
Myeloproliferative Neoplasms (MPN): To confirm diagnosis and monitor MPN and evaluate levels of JAK2, CALR and MPL mutations.
Lymphoma: Liquid biopsy and cfDNA analysis is recommended for patients with lymphoma and specific mutations. The levels of the detected mutations can be used to monitor these diseases and evaluate therapy. Analysis of the original diagnostic sample is required for proper and sensitive monitoring of lymphoma.
Clonal Hematopoiesis of Indeterminate Potential (CHIP): Distinguish CHIP from clinically active and relevant hematologic neoplasm based on an internally developed algorithm using variant allele frequency, chromosomal structural abnormalities, clinical and laboratory data and longitudinal data. This distinction is particularly important when evaluating minimal residual disease and in the presence of other neoplastic process.
Minimal Residual Disease (MRD): Our MRD testing can detect both tumor- informed and progression abnormalities. Additionally, the testing provides insights into chromosomal structural abnormalities via a molecular karyotype.
Turn Around Time: 5-7 days
- Peripheral blood: 5-10 mL. EDTA tube is preferred.
Specimen Preparation and Shipping Guidelines
Use the Hematology Transport Kit
- Complete Requisition, making sure all sections are completed in their entirety including client information, patient Information, specimen Information and test Selection. Missing information may delay reporting of test results.
- Diagnosis/patient history is extremely important in rendering the correct interpretation of results and should also be filled out as completely as possible. A copy of a Path report should be included.
- Ensure the specimen is labeled with patient name and number. A minimum of two patient identifiers is required for each specimen.
For blood samples:
- Ship using a cold pack. The cold pack should not directly contact the blood tube. Ship as soon as sample collected with overnight delivery.
Genes validated and tested for Mutations in DNA testing for hematology
| 1-40 | 41-80 | 81-120 | 121-160 | 161-179 |
|---|---|---|---|---|
| ABL1 | CDKN2A | HNF1A | NFKBIA | SMC1A |
| AKT1 | CDKN2B | HOXB13 | NOTCH1 | SMO |
| AKT2 | CDKN2C | HSP90AA1 | NOTCH2 | SOCS1 |
| AKT3 | CEBPA | IDH1 | NOTCH3 | SRC |
| ALK | CHEK1 | IDH2 | NPM1 | SRSF2 |
| AMER1 | CHEK2 | IGF1R | NRAS | STAG2 |
| APC | CIC | IKZF1 | NSD1 | STAT3 |
| ARID1A | CREBBP | IKZF3 | PALB2 | STK11 |
| ARID1B | CRLF2 | IRF4 | PAX5 | TERT |
| ARID2 | CSF1R | JAK1 | PBRM1 | TET2 |
| ASXL1 | CSF3R | JAK2 | PDGFRA | TGFBR2 |
| ATM | CTNNA1 | JAK3 | PDGFRB | TP53 |
| ATRX | CTNNB1 | KAT6A | PHF6 | TSC1 |
| B2M | CUX1 | KDM5C | PIK3CA | TSC2 |
| BCL2 | CXCR4 | KDM6A | PIK3R1 | TSHR |
| BCL2L1 | DDR2 | KDR | PIK3R2 | UBA1 |
| BCL6 | DICER1 | KEAP1 | PIM1 | WT1 |
| BCOR | DNMT3A | KIT | PLCG1 | ZNF217 |
| BCORL1 | EP300 | KMT2A | POLD1 | ZRSR2 |
| BCR | ERG | KMT2B | POLE | |
| BIRC3 | ETV6 | KMT2C | PPM1D | |
| BLM | EZH2 | KMT2D | PPP2R1A | |
| BRAF | FAM175A | KRAS | PTCH1 | |
| BRCA1 | FAM46C | MAP2K1 | PTEN | |
| BRCA2 | FANCA | MAP2K2 | PTPN11 | |
| BTK | FANCC | MAP2K4 | RAD21 | |
| CALR | FANCD2 | MAP3K1 | RAD50 | |
| CARD11 | FANCE | MAP3K14 | RAD51 | |
| CBL | FANCF | MAPK1 | RB1 | |
| CBLB | FANCG | MCL1 | RHOA | |
| CBLC | FAS | MDM2 | RNF43 | |
| CCND1 | FBXW7 | MDM4 | RUNX1 | |
| CCND3 | FLT3 | MEF2B | SDHB | |
| CD274 | GATA1 | MPL | SETBP1 | |
| CD79A | GATA2 | MRE11A | SETD2 | |
| CD79B | GATA3 | MTOR | SF3B1 | |
| CDH1 | GEN1 | MUTYH | SMAD2 | |
| CDK12 | GNAQ | MYC | SMAD4 | |
| CDK4 | GNAS | MYD88 | SMARCA4 | |
| CDK6 | H3F3A | NEF2 | SMARCB1 |
Request Kits
Fill out the form below to request kits. Please refer to the Specimen Requirements page for more details.
*GTC will need to set you up in our system if this is your first order.
GTC uses AI in every step of our analysis and it makes a difference in helping make a new discovery daily that improve patient care.
Once the data is offloaded from the sequencer, our AI:
- Assists with mutation analysis, identifying non-mutations and artifacts
- Compares various data sets to explore disease biology
- Provides support for clinical decision making and classification of the disease
- It helps with matching patients to therapeutics and presents clinical trial options
- Aggregates data for report generation and simplifies the results so they are easily understood
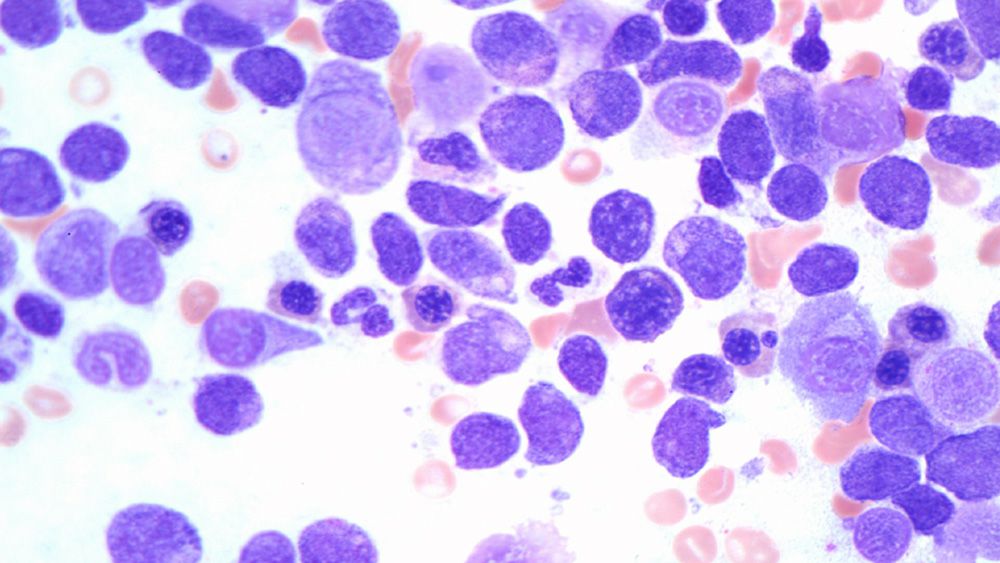
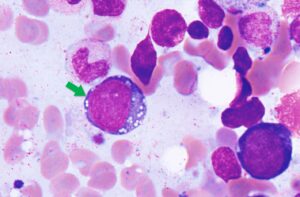
Case Study: VEXAS Syndrome
Background
VEXAS syndrome is a disease with inflammatory and hematologic (blood) manifestations. The syndrome is caused by mutations in the UBA1 gene affecting the Met41 residue of the protein and resulting in decreased cellular ubiquitylation activity and hyperinflammation. This is an adults-onset fatal disease that may present as myelodysplastic syndrome, aplastic anemia or multiple myeloma, but characterized by fevers, low white cell count, vacuoles in bone marrow cells, dysplastic bone marrow, pulmonary inflammation, chondritis, and vasculitis. Detecting UAB1 gene mutations in the is the only way for confirming the diagnosis of this disease.Clinical History
68-year-old male With low-grade myelodysplastic syndrome and inflammatory manifestations including arthritis, chondritis or other autoimmune disorders Molecular Profiling Findings Mutations in UBA1, DNMT3A, and TET2 genesDiscussion
The presence of DNMT3A, and TET2 suggest early low-grade myelodysplastic syndrome (MDS). And the detection of UBA1 mutation along with the patient’s symptoms confirmed the diagnosis of VEXAS. This patient was undiagnosed for long period of time and became transfusion dependent. By using any of our hematology DNA, DNA+RNA or cfDNA NGS panels; we are able to accurately diagnose VEXAS syndrome. This patient and most of the patients who are currently diagnosed with VEXAS have had numerous tests and tried multiple treatments. VEXAS should be considered in patients with systemic autoinflammatory disorders as well as patients with clinical presentation of myelodysplastic syndrome.Download PDF (VEXAS case study brochure)
References
1. David B. Beck, M.D., et al. Somatic Mutations in UBA1 and Severe Adult-Onset Autoinflammatory Disease N Engl J Med 2020; 383:2628-2638, DOI: 10.1056/NEJMoa2026834 2. James A. Poulter, et al. Novel somatic mutations in UBA1 as a cause of VEXAS syndrome. Blood (2021) 137 (26): 3676–3681. 3. Marcela A. Ferrada, et al. Somatic Mutations in UBA1 Define a Distinct Subset of Relapsing Polychondritis Patients With VEXAS, Arithritis & Rheumatology, doi.org/10.1002/art.41743.1. Rogers A, Joe Y, Manshouri T, Dey A, Jilani I, Giles F, Estey E, Freireich E, Keating M, Kantarjian H, Albitar M. Relative increase in leukemia-specific DNA in peripheral blood plasma from patients with acute myeloid leukemia and myelodysplasia. Blood. 2004;103:2799–801. 2. Nakamura S, Yokoyama K, Shimizu E, Yusa N, Kondoh K, Ogawa M, Takei T, Kobayashi A, Ito M, Isobe M, Konuma T, Kato S, Kasajima R, Wada Y, Nagamura-Inoue T, Yamaguchi R, Takahashi S, Imoto S, Miyano S, Tojo A. Prognostic impact of circulating tumor DNA status post-allogeneic hematopoietic stem cell transplantation in AML and MDS. Blood. 2019 Jun 20;133(25):2682-2695. doi: 10.1182/blood-2018-10-880690. 3. Paul Yeh, Michael Dickinson, Sarah Ftouni, Tane Hunter, Devbarna Sinha, Stephen Q. Wong, Rishu Agarwal, Ravikiran Vedururu, Kenneth Doig, Chun Yew Fong, Piers Blombery, David Westerman, Mark A. Dawson and Sarah-Jane Dawson. Molecular disease monitoring using circulating tumor DNA in myelodysplastic syndromes. Blood. 2017;129(12):1685-1690. 4. Albitar A, Ma W, DeDios I, Estella J, Ahn I, Farooqui M, Wiestner A, Albitar M. Using high-sensitivity sequencing for the detection of mutations in BTK and PLCγ2 genes in cellular and cell-free DNA and correlation with progression in patients treated with BTK inhibitors. Oncotarget. 2017 Mar 14;8(11):17936-17944. doi: 10.18632/oncotarget.15316. PMID: 28212557 5. Albitar F, Ma W, Diep K, De Dios I, Agersborg S, Thangavelu M, Brodie S, Albitar M. Deep Sequencing of Cell-Free Peripheral Blood DNA as a Reliable Method for Confirming the Diagnosis of Myelodysplastic Syndrome. Genet Test Mol Biomarkers. 2016 Jul;20(7):341-5. doi: 10.1089/gtmb.2015.0278. PMID: 27248906 6. Aljurf M, Abalkhail H, Alseraihy A, Mohamed SY, Ayas M, Alsharif F, Alzahrani H, Al-Jefri A, Aldawsari G, Al-Ahmari A, Belgaumi AF, Walter CU, El-Solh H, Rasheed W, Albitar M. Chimerism Analysis of Cell-Free DNA in Patients Treated with Hematopoietic Stem Cell Transplantation May Predict Early Relapse in Patients with Hematologic Malignancies. Biotechnol Res Int. 2016;2016:8589270. doi: 10.1155/2016/8589270. 7. Ma W, Kantarjian H, Zhang X, Jilani I, Sheikholeslami MR, Donahue AC, Ravandi F, Estey E, O’Brien S, Keating M, Giles FJ, Albitar M. Detection of nucleophosmin gene mutations in plasma from patients with acute myeloid leukemia: clinical significance and implications. Cancer Biomark. 2009;5(1):51-8. doi: 10.3233/CBM-2009-0583. PMID: 19242062 8. Yeh CH, Tseng R, Albitar M. Plasma-based detection of clonality in lymphoid malignancies. Eur J Haematol. 2009 Jun;82(6):450-3. doi: 10.1111/j.1600-0609.2009.01231.x. PMID: 19187275. 9. Ma W, Kantarjian H, Zhang X, Sun W, Buller AM, Jilani I, Schwartz JG, Giles F, Albitar M. Higher detection rate of JAK2 mutation using plasma. Blood. 2008 Apr 1;111(7):3906-7. doi: 10.1182/blood-2008-02-139188. PMID: 18362222. 10. Giles FJ, Albitar M. Plasma-based testing as a new paradigm for clinical testing in hematologic diseases. Expert Rev Mol Diagn. 2007 Sep;7(5):615-23. Review. PMID: 17892367. 11. Ma W, Tseng R, Gorre M, Jilani I, Keating M, Kantarjian H, Cortes J, O’Brien S, Giles F, Albitar M. Plasma RNA as an alternative to cells for monitoring molecular response in patients with chronic myeloid leukemia. Haematologica. 2007 Feb;92(2):170-5. PMID: 17296565. 12. Ma W, Kantarjian H, Jilani I, Gorre M, Bhalla K, Ottmann O, Giles F, Albitar M. Heterogeneity in detecting Abl kinase mutations and better sensitivity using circulating plasma RNA. Leukemia. 2006 Nov;20(11):1989-91. Epub 2006 Aug 24. PMID: 16932346. 13. Ma W, Jilani I, Gorre M, Keating M, Chan H, Tseng R, Kantarjian H, O’Brien S, Giles FJ, Albitar M. Plasma as a source of mRNA for determining IgV(H) mutation status in patients with chronic lymphocytic leukaemia. Br J Haematol. 2006 Jun;133(6):690-2. 14. Jilani I, Estey E, Manshuri T, Caligiuri M, Keating M, Giles F, Thomas D, Kantarjian H, Albitar M. Better detection of FLT3 internal tandem duplication using peripheral blood plasma DNA. Leukemia. 2003 Jan;17(1):114-9. 15. Kurtz DM, Green MR, Bratman SV, Scherer F, Liu CL, Kunder CA, Takahashi K, Glover C, Keane C, Kihira S, Visser B, Callahan J, Kong KA, Faham M, Corbelli KS, Miklos D, Advani RH, Levy R, Hicks RJ, Hertzberg M, Ohgami RS, Gandhi MK, Diehn M, Alizadeh AA.Noninvasive monitoring of diffuse large B-cell lymphoma by immunoglobulin high-throughput sequencing. Blood. 2015 Jun 11;125(24):3679-87.
How to complete the Genomic Testing Cooperative requisition form.
Download our
Test Requisition
Keep in mind that we do not accept blood samples directly from individuals. Talk with your M.D. to fill out the form for you.
Do You Want to Download the Sample Report?